Brain Injury Awareness Month: Our Perspective on TBIs
March is Brain Injury Awareness Month, and we wanted to dive deeper into one of the most common invisible wounds – traumatic brain injury or TBI – to give a better picture of what it is and the often times life-altering effects, including the potential for suicide.
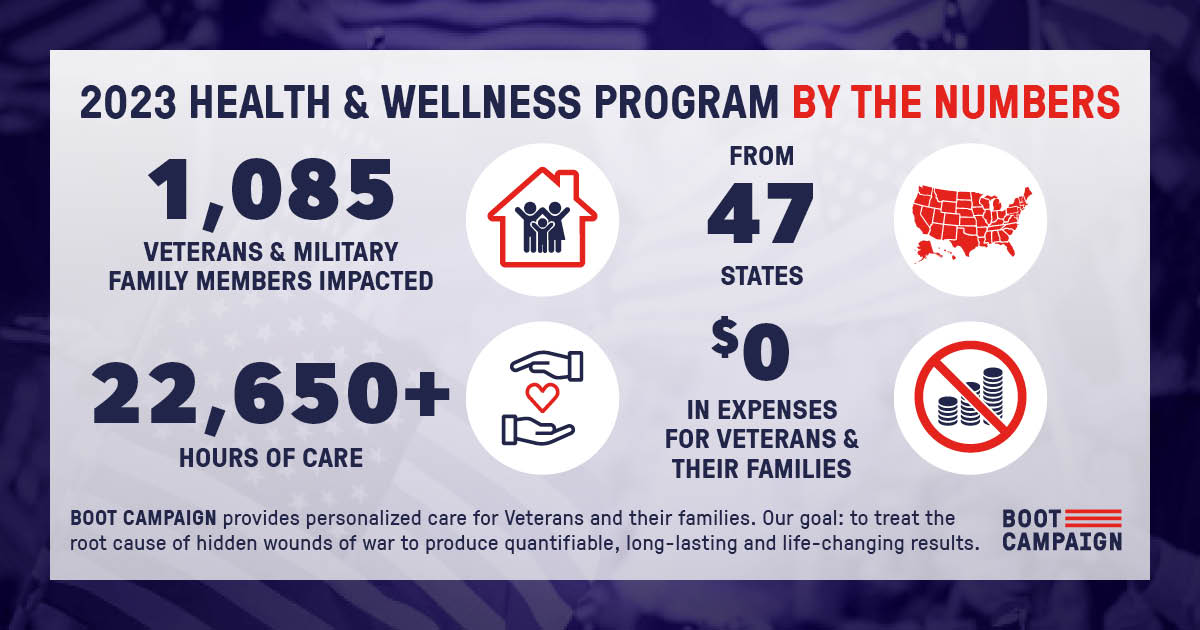
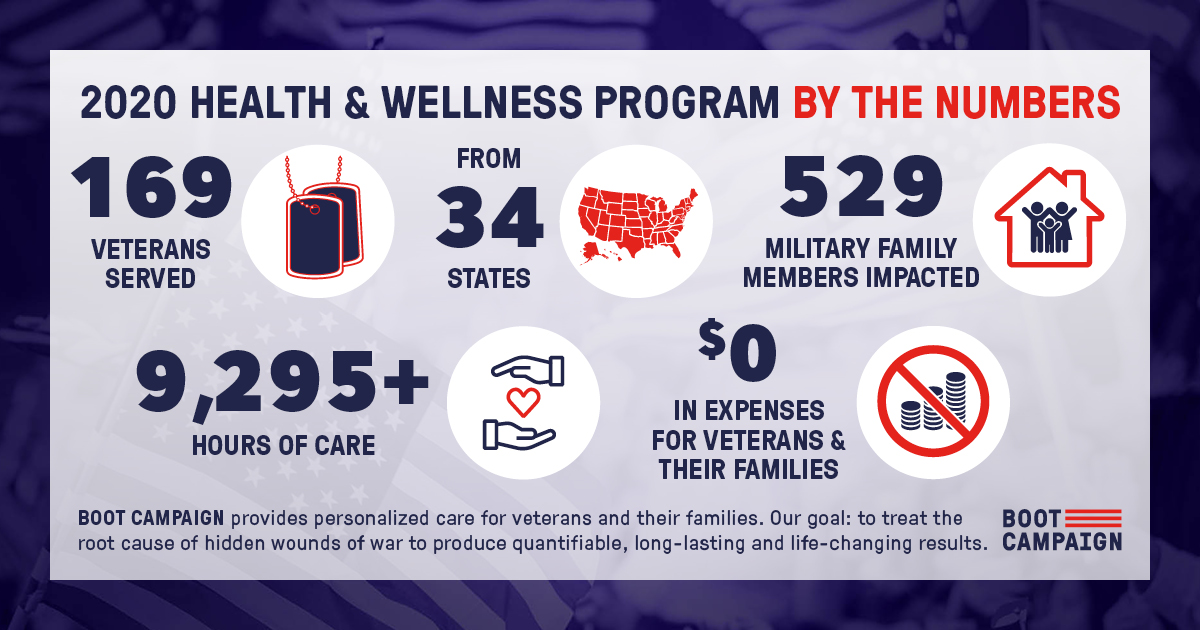
At Boot Campaign, we support veterans who are struggling with invisible wounds of war, including traumatic brain injury and posttraumatic stress, by providing individualized care and treatment that they need and deserve at no cost to them. We want veterans to know that their service and sacrifice matters and, most importantly, that hope exists to not only treat brain injury, but to effectively heal the root cause of many symptoms that accompany them in order to prevent suicide and other types of long-term outcomes that plague the military community.
Since 2000, more than 490,000 U.S. service members have been diagnosed with a brain injury. More than 83% of those 490,000 are classified as “mild” and roughly 60,000 are labeled as “moderate” or “severe.” But no matter the classification, any TBI can result in difficulties with sleep, memory, and headaches months, even years, later.
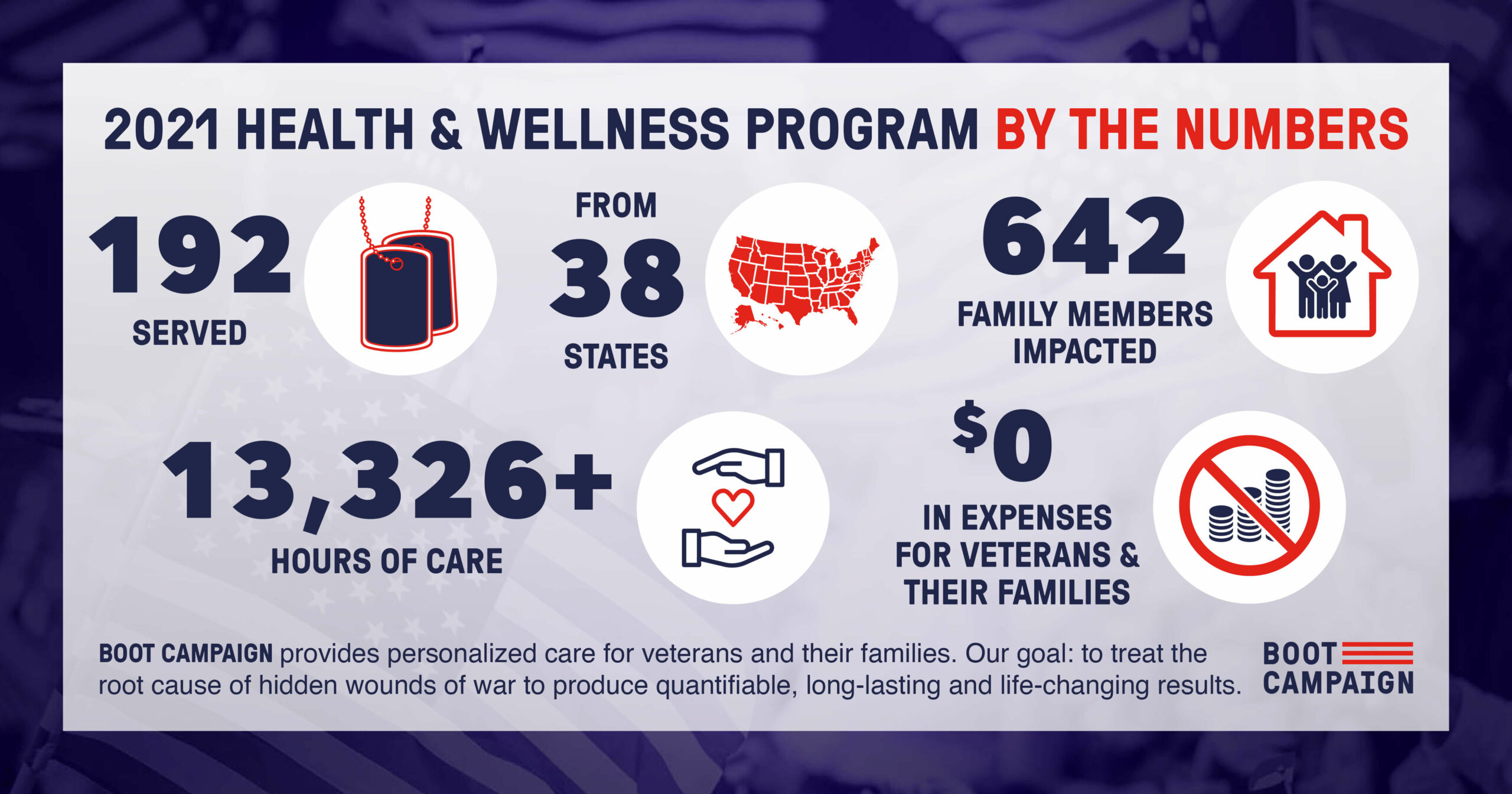
TBIs are considered to be a signature wound of the Iraq and Afghanistan wars, as thousands of troops received one or more as the result of roadside bomb blasts, explosives training and combat action, shelling and weapons firing. TBIs fall along a spectrum from concussion, known also as a mild brain injury, to severe with significant brain damage. While we know not every individual exiting or still in military service suffers from this type of invisible wound, among the veterans served through our Health & Wellness program in 2021, 68% reported having experienced at least one TBI.
Another often referenced invisible wound is posttraumatic stress (PTS). PTS and TBI often coexist and have overlapping symptoms; furthermore, many brain injuries, and especially moderate-to-severe brain injuries, are often sustained during traumatic experiences which only compounds the problem. Of the veterans who participated in our program in 2021, 85% reported struggling with PTS and 61% experienced a combination of both TBI and PTS. The similar symptoms between these two invisible wounds can make diagnosis and treatment difficult as medical professionals work to tease out the symptoms and causes of each. That is why our team at Boot Campaign takes the time to look at the brain and body of each veteran and provide the treatment they need individually through holistically-based care.
The consequences of minimizing the severity and importance of invisible wounds can be devastating. A recent study published in the Journal of Head Trauma Rehabilitation suggests that veterans with moderate TBI are more than twice as likely as those without a TBI to die by suicide.
However, research has shown that our brains have the capacity to change and even heal from damage sustained over the course of a lifetime given the right interventions and right environment. Through therapy, coaching and cutting-edge treatments, veterans suffering from traumatic brain injuries can make improvements by relearning and rewiring new pathways in their brain.
Of course, everyone’s exposures and experiences are different, thus the type, duration, and outcome of rehabilitation will be different for everyone based on the severity of and length of time since the injury and areas of the brain impacted. While our team at Boot Campaign is here to assist veterans with brain injury that qualify for our program, there are also various other organizations that exist to help those with more severe injuries or those with degenerative brain disease caused by brain injuries.
Bottom line: It is our position as an organization, led by clinically and culturally competent mental health professionals, including a licensed clinical psychologist, in collaboration with various other specialties to include neurologists and psychiatrists, that breaking down barriers to seeking care is of utmost importance. Our goal is to show veterans that whatever label or diagnosis they carry does not have to be a life-long affliction without hope.
*Original Blog Written in 2022 with updated stats edited in Feb. 2024.