SHATTERING STIGMA OF SEEKING CARE FOR MENTAL HEALTH | PART II

PART TWO OF A TWO PART SERIES
In our first conversation with veterans Kelly Rodriguez and Spencer Milo we addressed the issue of stigma and some the challenges warriors face when working to overcome hidden wounds of war. We would be remiss if we looked solely at the active duty service member or veteran and not their entire family unit.
In the second installment of this series dedicated to continuing the conversation about mental health and suicide in the military community all year, we’ll continue our conversation with Kelly Rodriguez — veteran, military spouse and military mom — as well as Roxana Delgado, Ph.D., health scientist and the wife of US Army retired Sergeant First Class Victor L. Medina. SFC(Ret.) Medina is a combat wounded Veteran and Purple Heart Recipient. Both share their thoughts on how hidden wounds affect spouses, caregivers and military children who serve alongside their parents.
Shelly: Firstly — thank you both for your service to our great nation and for taking the time to address these important issues. I’d love to know your point of view about how stigma surrounding mental health in the military affect families/caregivers?
Kelly: Clearly it adds stress to the family in general. As a caregiver, it is difficult knowing that there is something going on with your loved one and you can’t fix it. You can’t push too hard and only offer support.
Roxana: This is a loaded question! It affects the family in so many aspects, but especially the social component. Military children are the most affected since they can’t live the normal experiences children typically have, like sleepovers, gatherings, birthdays, etc. The spouse/parent is also affected by stigma when stepping into the caregiver role, given the lack of understanding from employers, friends and family. It seems there is lack of knowledge and understanding about caring for a loved one with brain illness. The tasks and responsibilities may differ from taking care of a loved one with a physical disability, yet it may be equally time consuming and requires a lot of effort. For example, caring for someone with psychosis or suicidal thoughts may be physically and emotionally exhausting. These are aspects that are not well understood in the community and applies to military and non-military settings. One of the biggest examples is the comparison of a hospitalization following a suicide attempt versus an auto accident. Who receive the most cards and sympathetic messages?
Shelly: How has your journey to overcome hidden wounds of war impacted your family life now?
Kelly: We are still on this journey to be honest. I am no longer self-medicating with alcohol, which is a positive for my family as a whole. The hard part, though, is that I no longer have a way of “hiding” how I’m feeling. I have to face and deal with things head on, versus self-medicating or lashing-out. Since seeking treatment, I am happier and think more clearly; I am a better wife and mother since I started this journey. This is the best way for me to live my best life.
Roxana: In our family, we have been incredibly impacted by traumatic brain injury (TBI). On June 29th it will be 10 years since my husband was wounded by an explosive formed projectile in Iraq. The acquired disabilities were new to us. We stepped into a new lifestyle unknown to us. Our new life had new demands and posed challenges never experienced before. One of them was at the beginning of our journey, we encountered a healthcare system with limited knowledge about brain injuries, especially those resulting from explosions, better known as blast-induced TBI. The medical system did not have guidelines or a standard of care to treating closed head TBIs. Despite the evidence of hemorrhage there was no treatment plan for closed head moderate TBI in place. My husband’s treatment plan required an interdisciplinary approach and ensuring he received this level of care was the most challenging tasks at the beginning of our journey.
My personal journey redefined the goals of our family life. We were a typical married couple, each working on our own careers, his in the military, mine as a health scientist. Little did we know that our journey would collide and that our strengths would be fused to a common goal, seeking to improve the lives of people with disabilities resulting from a brain injury. Up to 10 years ago our plans included our careers, living as a military family and having the satisfaction of serving our nation. We were devoted and committed to the mission. In 2009 our mission was redefined and our new mission was LIVING (not surviving) post-injury. We changed our hobbies, especially what we loved the most, our motorcycle rides on the weekends. We were challenged in many ways, but we lived and we continue to live, love and we enjoy very much every aspect of our journey. Our experiences helped shape new policies regarding brain injuries, and it gave us the motivation to continue to serve our community.
Q: Kelly, you and your husband are not only veterans and veterans who have been candid in sharing your struggles and successes overcoming hidden wounds of war, but you are also the parents of someone still serving. How do you talk about your mental health and the need to prioritize it to your active duty son?
Kelly: My husband and I were both honest with him about PTSD. It is a reality of war and service. I wanted him to know that asking for help is a sign of strength and courage and that these reactions to war are normal. Early treatment helps. I also hope that his experience with us as parents allows him to help his buddies in his unit. Like any other injury, if you aren’t taking care of yourself, it is very hard to take care of others.
Q: What would you say to a military spouse/caregiver about their veteran who is dealing with hidden wounds?
Kelly: The first thing I’d say is this is a wound you can’t heal for your veteran. It is hard as a caregiver to accept that you can’t fix it for them; it’s what caregivers do…fix things. In the case of hidden wounds, you can support, encourage and most importantly, give your veteran space when they need it. When you suspect that things are going in a bad direction, reach out to your veterans support network. Oftentimes, veterans are more inclined to listen to a friend or mentor.
Roxana: I believe that a spouse/caregiver dealing with hidden wounds must be equipped with sufficient knowledge to know what to expect and how to best handle their circumstances. But how do you do this?
- Education: Expanding education about the medical condition will help the caregiver be successful at advocating for their care recipient at the same time it will help with their family wellbeing. Hidden wounds aren’t a one size fits all. Find solutions that will fit your family and always strive to improve their wellbeing. Hidden wounds aren’t always cured, actually, most of the time cure should not be the goal. Learning to mitigate the effects may improve the overall health and quality of life.
- Get connected: Identify organizations serving military caregivers and connect with their resources. These days there are a number of national and local organizations serving caregivers. It is important to identify our own unique needs and be open to receiving assistance.
- Don’t lose yourself: Remember that you are a unique person, with a set of characteristics that makes you who you are. Strive to retain the core of what makes up your unique identity, so in other words… who you are. Caregiving is a role but it should not be an identity. Strive to accommodate the role of caregiving in the space of your life in a way that you can continue to live, dream and achieve. Do not allow circumstances to stop you. Some goals may need to be redefined but never lose sight of purpose and goals.
- Faith/Spirituality: Often we focus on all the aspects of health, but strengthening one’s faith and keeping a healthy spiritual life is beneficial. In my personal experience, faith is the component that has kept us alive and living a fulfilled life. It is everything to me.
Shelly: Again, thank you both for your perspective, insight and willingness to share your experiences both as a military spouse and military family. We are grateful.
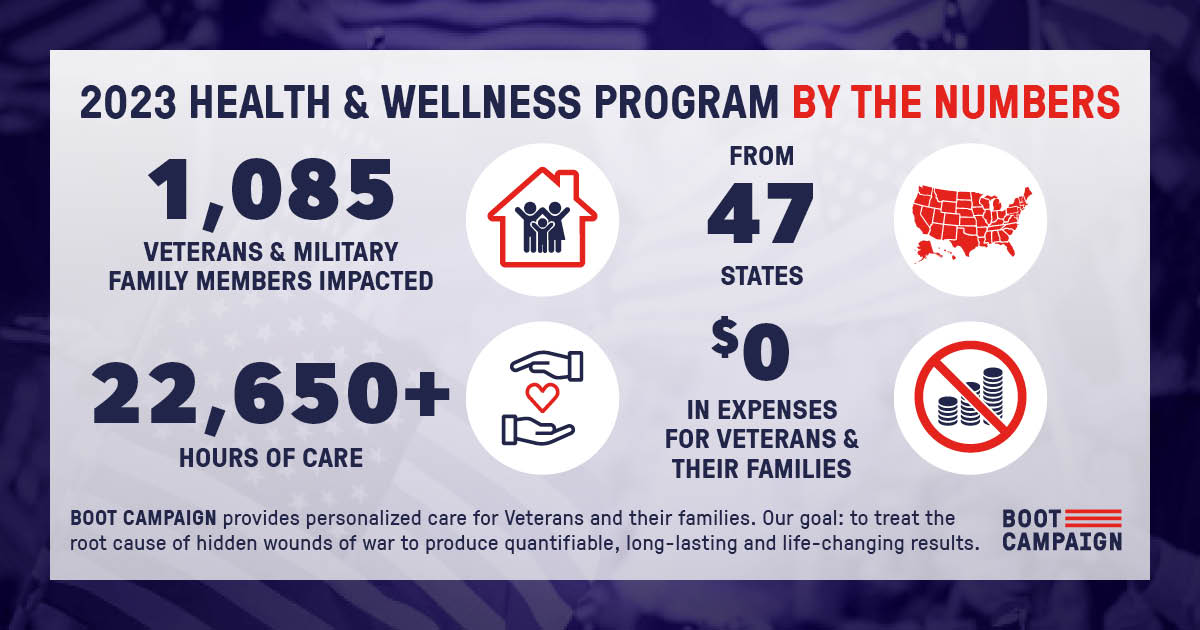
At Boot Campaign, we want to do more than just make Americans aware about the challenges of military service. We aim to educate about the long-term effects of war and actively provide access to treatment to overcome those issues. We know that since 2001, more than 2.8 million servicemen and women have been deployed around the world.
- One in three will develop post-traumatic stress disorder (PTSD);
- One in five will suffer a traumatic brain injury (TBI), and
- One in ten will experience a substance use disorder.
What’s more, treatment costs are 7X higher for veterans with complex diagnoses such as PTSD and TBI than those who suffer from physical wounds alone and less than 50% of military personnel and veterans who experience invisible wounds receive care. We are a nation at war and for the foreseeable future, war will continue. That means there will be more and more veterans, more soldiers, sailors, airmen, Marines, Coast Guardsmen, National Guardsmen and Reservists who need our help. We owe it to all members of the Armed Forces and the more than 22 million veterans who call America home, to live laced up in support of their service and sacrifice while they wear the uniform and when they take it off and return to civilian life. The men and women of the U.S. Armed Forces and their families are our fellow Americans. They are mothers, fathers, wives, husbands, brothers, sisters, children and friends. Let’s live laced up for them.